


View all photos
Nursing Home Gallery













Amenities for Aaron Manor Nursing & Rehabilitation
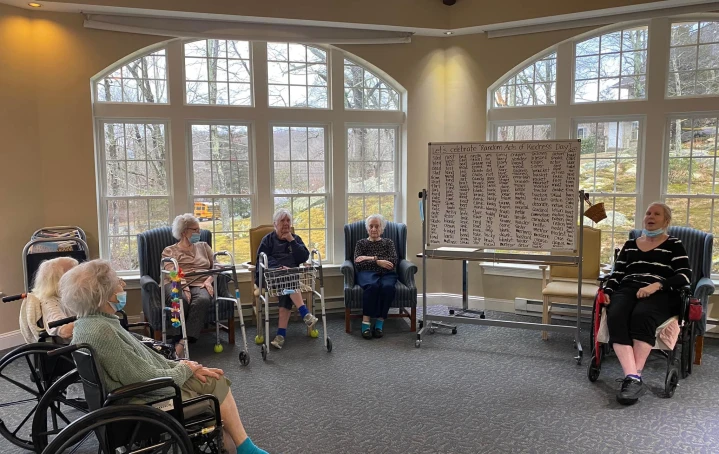
activities
cultural devotional services
Bible Study Group
Catholic Services
Christian Services
Other Religious Services
Protestant Services
Visiting Chaplain or Priest
educational classes
Art Classes
entertainment
Live Musical Performances
exercise
Group Therapy
games clubs
Current Events Club
Gardening Club
other
Activities On-site
Intergenerational Programs
parties celebrations
BBQs or Picnics
Birthday Parties
Dances
pets
Pet-focused Therapy Programs
community amenities
common areas
Beauty Salon
Garden
Central Fireplace
Computer or Media Center
Indoor Common Areas
Library
Meeting Room
Outdoor Common Areas
Outside Patio
Private Bath
TV Lounge
dining
Private Dining Room
languages spoken
English
Filipino
French
Italian
Polish
Spanish
Electronic Language Interpreter
memory care
Indoor Walking Paths
Wander Guard or Similar System Available
pets
Cats Allowed
Dogs Allowed
recreational areas
Fitness Center
Piano or Organ
Raised Garden Beds
Rehab Gym
services
Housekeeping
Laundry Service / Drycleaning
smoking
Smoke Free Environment
transportation parking
Property Convenient to Public Transit
Resident Parking Available
Transportation at Cost
dining
dietary accommodations
Gluten-free
Low / No Sodium
No Sugar
Vegetarian
dining services
Chopped Meals
Guest Meals
Meals Provided
Professional Chef
Pureed Meals
Restaurant Style Dining
healthcare services
diabetic care
Diabetic Care
high acuity care
Catheter Care
Feeding Tube
History of Psychiatric Care
IV Care
Oxygen
Wound Care
Tracheostomy Tube
Cardiac Management Program
Total Parenteral Nutrition (TPN)
Stroke Recovery
Pulmonary Care
Parkinson’s Care
incontinence care
Bowel Incontinence
Reminders
Urinary Incontinence
medication management
Full Medication Management Available
Licensed Nurses May Administer Injections with Doctor's Order
Medication Aides May Administer Injections with Doctor's Order
Reminders and Monitoring Available
Pharmaceutical Delivery Service
memory care
Sensory-based Programs
Redirection, Cuing, Disorientation
other
24 hours a day
Total Transfer / Hoyer Lift
Staff May Administer Insulin Injections
staffing ancillary services
24-Hour Awake Staff
Activity Director
Behavioral Health Services
Doctor on Call
Home Care Agency On-Site
Hospice Available On-Site
On-site Medical Director
On-site Nurse Practitioner
Medication Care Managers / Medication Technicians
Nutritionist / Dietician
Optometrist
Dental Care
Registered Nurses
Occupational Therapy
Physical Therapy
Podiatry Care
Speech Therapy
Palliative Care
Rehabilitation Therapy
Discharge Planning
Case Management
Outpatient Rehabilitation Services
Orthopedic Rehabilitation
Inpatient Care
Outpatient Care
Bariatric Specialties
Colostomy Care
Restorative Care
Music Therapy
Physiatry Services
Psychiatric Services
X-ray
Recreational Therapy
Telemedicine
Pain Management
Laboratory Services
Social Worker
Respiratory Therapy
Occupational Therapy offered 7 days a week
Respiratory Therapy offered 7 days a week
Neurological Care
Infectious Disease Care
Individualized Care Plans
room amenities
bathroom
Wheelchair Accessible Showers
Private Bathroom
other
Air Conditioned
Individual Climate Control
utilities
Cable or Satellite TV
Wi-Fi/high-speed internet
Your review of Nursing home name
Important info!
If you are either a resident, or family/friend of a resident, please share your insights and experiences in as much detail as
possible to help others learn more about this facility.
Please note we cannot accept your review if you work at this facility, or if you have a professional connection to this facility
(e.g. a visiting doctor or hairstylist).
Please note we cannot accept your review if you have only toured this facility, you must be connected to a resident to leave
a review.
Please note this is not a formal complaints procedure, and nursinghomes.com does not license, oversee or regulate nursing
homes. For complaints about Facilities, we encourage you to contact the Facility directly.

